Normal Kidney function
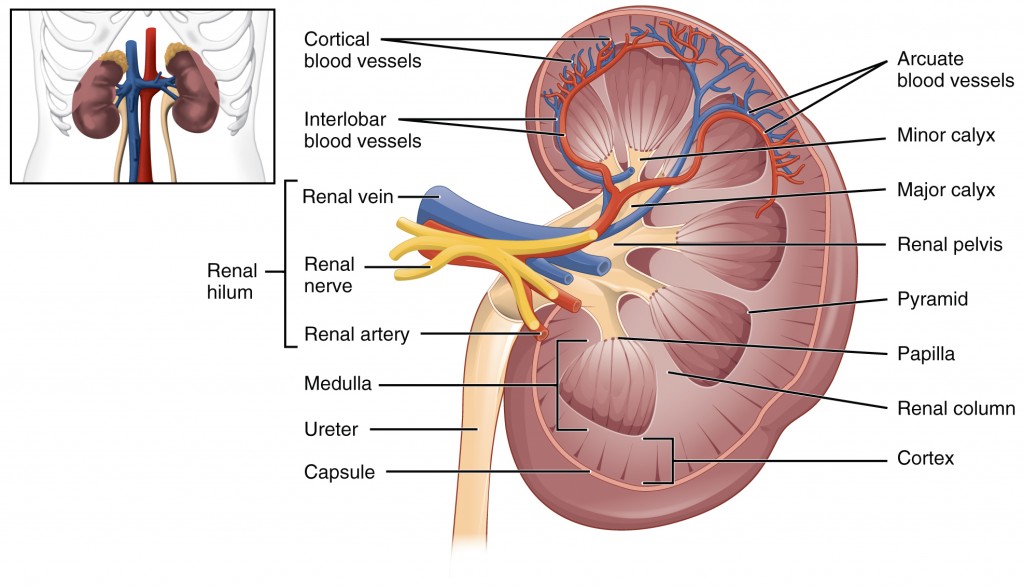
The kidneys remove wastes and excess water from the blood. They also control the balance of sodium, potassium, phosphorus, calcium and other chemicals in the body. Filtering process is done in the kidney through structures called nephrons. Wastes and fluids are combined to form urine which is eliminated through the kidneys. Normally each kidney has approximately 1 million of nephrons. Damage to those units result in chronic kidney disease.
What is creatinine?
Creatinine is a waste product that comes from muscle metabolism and is excreted by the kidneys. Everyone has creatinine in the bloodstream and it is not a toxic substance. Usually higher than normal creatinine level indicates poor kidney function that requires evaluation. Blood urea nitrogen (BUN) is a measure of protein metabolism and if elevated can also indicate kidney damage since it is eliminated by the kidneys. BUN level can vary based on fluid intake, diet and use of various medications. Urinalysis is a test examining the urine that can detect protein, blood and glucose suggestive of kidney disease
What is GFR?
GFR stands for Glomerular Filtration Rate. It is calculated by the mathematical formula using body weight, serum creatinine, patient’s age and gender. It is a measure of the level of kidney function. GFR determines the stage of kidney disease and helps to design a treatment plan. A low GFR is a sign of severe kidney damage and might need to be treated with dialysis. Early detection of kidney damage gives the doctor a better chance to slow the progression of renal disease or to cure it.
Stages of kidney injury
In 2002, the National Kidney Foundation’s Kidney Disease Outcomes and Quality Initiative (K/DOQI) developed a staging process for chronic kidney disease (CKD) based on glomerular filtration rate (GFR).
| Stage I | GFR > 90 ml/min | 5,900,000 patients in the US |
| Stage II | GFR 60-90 ml/min | 5,300,000 patients |
| Stage III | GFR 30-60 ml/min | 7,600,000 patients |
| Stage IV | GFR 15-30 ml/min | 400,000 patients |
| Stage V | GFR <15 ml/min | 70,000 patients |
What are the warning signs of kidney disease?
Kidney disease usually affects both kidneys. When kidney function gets weaker, waste products and fluids can build up in the body. Kidney failure might not cause any warning signs and symptoms for a long time. The determination about how good is the kidney function is made by the blood work ordered by the primary care physician. Patients with elevated BUN and creatinine are usually referred to a nephrologist for further evaluation. Some warning signs of renal disease might include elevated blood pressure, swelling of the legs, arms and puffiness around the eyes, frequent urination and foam in the urine, poor appetite, nausea and vomiting. These symptoms are associated with elevated BUN, creatinine, blood and or protein in the urine.
Certain medical conditions like diabetes mellitus, hypertension, family history of kidney disease, obesity, smoking can increase a risk of developing CKD (Chronic Kidney Disease).
Can kidney disease be treated?
Kidney disease can be treated successfully. Patients are usually evaluated by the nephrologist and a set of blood and urine tests are ordered. They also frequently have renal ultrasound ordered to assess kidney size. Occasionally renal biopsy might be needed when a small kidney sample is obtained using a tiny needle. That helps to make a final diagnosis and estimate prognosis and chance of recovery. The first step in the treatment of CKD is to determine the underlying cause. Multiple medications are available to treat kidney disease and the selection of treatment is frequently based on biopsy results. When treatment is not successful or kidneys are damaged before treatment is started some patients might require dialysis.
Acute kidney injury (AKI) is a sudden inability of the kidneys to perform their function. This can result in accumulation of excess fluids, salts, and waste in the body. This condition can develop quickly over the course of a few hours or days. AKI typically occurs due to an injury, illness or as a side effect of certain medications. AKI can occur in a patient with normal kidney function or in someone who already has chronic kidney disease. Treatment of acute kidney injury can frequently results in improvement of renal function but can also be irreversible leading to residual renal damage.
Chronic kidney disease (CKD).
Chronic kidney disease can develop slowly over many years and is often due to diabetes or hypertension. It can also be caused by other underlying chronic diseases or from severe acute kidney injury. More than 20 million Americans may have chronic kidney disease and many more are at risk. The major risk factors for chronic kidney disease are diabetes, high blood pressure, cardiovascular disease, and a family history of kidney disease. In Stages I and II kidneys might still function well, patients might not experience any symptoms, and prognosis is relatively good.>/p>
In stage III chronic kidney disease renal function continues to deteriorate leading to a buildup of waste products. Most of the patients do not have any symptoms. They have to be followed and monitored regularly by nephrologists to prevent further damage of the kidneys. Treatment consists of a good blood pressure and blood glucose control in diabetic patients, avoidance of NSAIDS, intravenous contrast exposure, smoking cessation, losing weight and low salt diet. Patients might be able to prevent progression of chronic kidney disease into later stage of disease.
In stage IV and V of chronic kidney disease waste products builds up to high levels that can make patients feel sick. Patients need to be followed by a nephrologist who will design appropriate treatment plan and might need to prepare you for dialysis treatement.
What are the symptoms of kidney failure?
Typical symptoms are increase fatigue, nausea and vomiting, loss of appetite and metallic taste in the mouth, swelling, shortness of breath, skin itching, tremors, change in urination and trouble concentrating.
Kidney biopsy
In some patients with kidney disease, the nephrologist might suggest to perform a kidney biopsy. This procedure is done in the radiology department under a local anesthesia where a small sample of the kidney tissue is obtained and examined under the microscope. A biopsy identifies a specific cause of kidney disease, helps to identify how much permanent damage has been done, and helps to assess renal prognosis.
Chronic kidney disease treatment.
Research shows that management of CKD is best done by nephrologists, specialists in treatment of kidney diseases. The first step in the treatment of CKD is to determine the cause. Some reversible causes of renal disease include impaired blood flow to both kidneys, blockage of urinary tract and the use of medications that can impair kidney function. It is important to treat hypertension since elevated blood pressure leads to further renal damage. A lot of patients with CKD have anemia. Some of them might require iron supplementation and Erythropoetin injection to increase production of the red blood cells. Patients with kidney disease might have elevated phosphorus levels and need to reduce phosphorus in their diet to lower the phosphorus blood level. Low potassium diet might be needed since CKD patients might develop high blood potassium level. Low salt diet might be needed to better control blood pressure. Dietary protein restriction is generally not advised as risk of low protein diet might outweigh benefits.
What can I do to protect my kidney?
Please avoid routine or frequent use of non-steroidal anti-inflammatory drugs (NSAIDS), commonly thought of as Advil, Motrin or Aleve. These include: Celecoxib (Celebrex), Diclofenac (Arthrotec, Voltaren), Etodolac (Lodine), Ibuprofen (e.g. Advil, Motrin), Indomethacin (Indocin), Meloxicam (Mobic), Nabumetone (Relafen), Naproxen (e.g. Aleve, Naprosyn), Oxaprozin (Daypro), Piroxicam (Feldene), Sulindac (Clinoril), and Aspirin. The selective COX-2 inhibitors like Celebrex are also NSAIDS and can cause renal damage. Acetaminophen (e.g. Tylenol) is safe to be used in patients with a kidney disease. Also try to avoid intravenous exposure to iodine-based contrast that is used for imaging studies like computerized tomography (CT) scans and angiograms since they can make kidney function worse. Non-contrast alternatives may be available. If an IV contrast procedure must be done, please let us know since certain interventions might protect your kidneys from contrast-induced kidney disease. If you have advanced renal disease (GFR less than 30) you should avoid gadolinium-based intravenous contrast dye, commonly used in magnetic resonance (MRI/MRA) studies. Gadolinium contrast has been associated with a rare but serious condition of thickening and hardening of the skin and organs called nephrogenic systemic fibrosis. Remember that the dose of some of the medications that you are using might need to be adjusted in patients who have CKD. Please bring the list of all of your medications including over the counter and herbal or natural remedies, to your medical appointments.
Anemia of chronic kidney disease
Hemoglobin is the protein in red blood cells that carry oxygen to tissue in our body. Low level of hemoglobin is called anemia and can occur at any stage of kidney disease. The risk of developing anemia increases as kidney disease worsens. The kidney normally secretes a glycoprotein called erythropoietin. Erythropoietin stimulates cells in the bone marrow to form into red blood cells. In patients with chronic kidney disease, the production of erythropoietin is lower which can lead to anemia. Anemia can manifest itself as weakness, shortness of breath, chronic fatigue, poor appetite, difficulty sleeping, dizziness, depression but can also be asymptomatic. Iron deficiency, vitamin deficiency, poor nutrition or inflammation can all contribute to anemia. Patients might benefit from administration of erythropoietin in injection form together with iron and vitamin supplements to stimulate red blood cell production and treat anemia related symptoms.